Are Human and Bovine Insulin Exactly Alike?
In the realm of diabetes treatment, insulin has long been hailed as a life-saving therapy, enabling millions of individuals to manage their blood sugar levels and mitigate the potentially severe complications of this chronic condition. However, as our understanding of insulin has deepened, a crucial question has emerged: Are insulin derived from humans and cows exactly alike?
To fully grasp the nuances of this inquiry, it is essential to understand the fundamental nature of insulin itself. This remarkable hormone, produced by specialized cells within the pancreas, plays a pivotal role in regulating blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells, where it can be utilized as an energy source or stored for future use.
The discovery of insulin as a treatment for diabetes dates back to the early 20th century when researchers Frederick Banting and Charles Best successfully isolated and purified the hormone from the pancreas of dogs and cattle. This groundbreaking achievement paved the way for the widespread use of insulin therapy, saving countless lives and revolutionizing the management of diabetes.
For many years, insulin derived from animal sources, primarily cows and pigs, served as the primary treatment option for people with diabetes. While these animal-derived insulins were effective in managing blood sugar levels, they were not identical to human insulin. Subtle differences in the amino acid sequences and structural configurations of these insulins contributed to varying degrees of efficacy, immunogenicity (the ability to trigger an immune response), and potential side effects.
As our understanding of molecular biology and biotechnology advanced, scientists embarked on a quest to produce human insulin through recombinant DNA technology. This pioneering approach involved introducing the human insulin gene into bacteria or yeast cells, allowing these microorganisms to produce human insulin molecules identical to those naturally produced by the human body.
The introduction of recombinant human insulin in the 1980s marked a significant milestone in diabetes treatment. By eliminating the need for animal-derived insulin, this synthetic human insulin offered several advantages, including reduced immunogenicity, improved efficacy, and potentially fewer side effects.
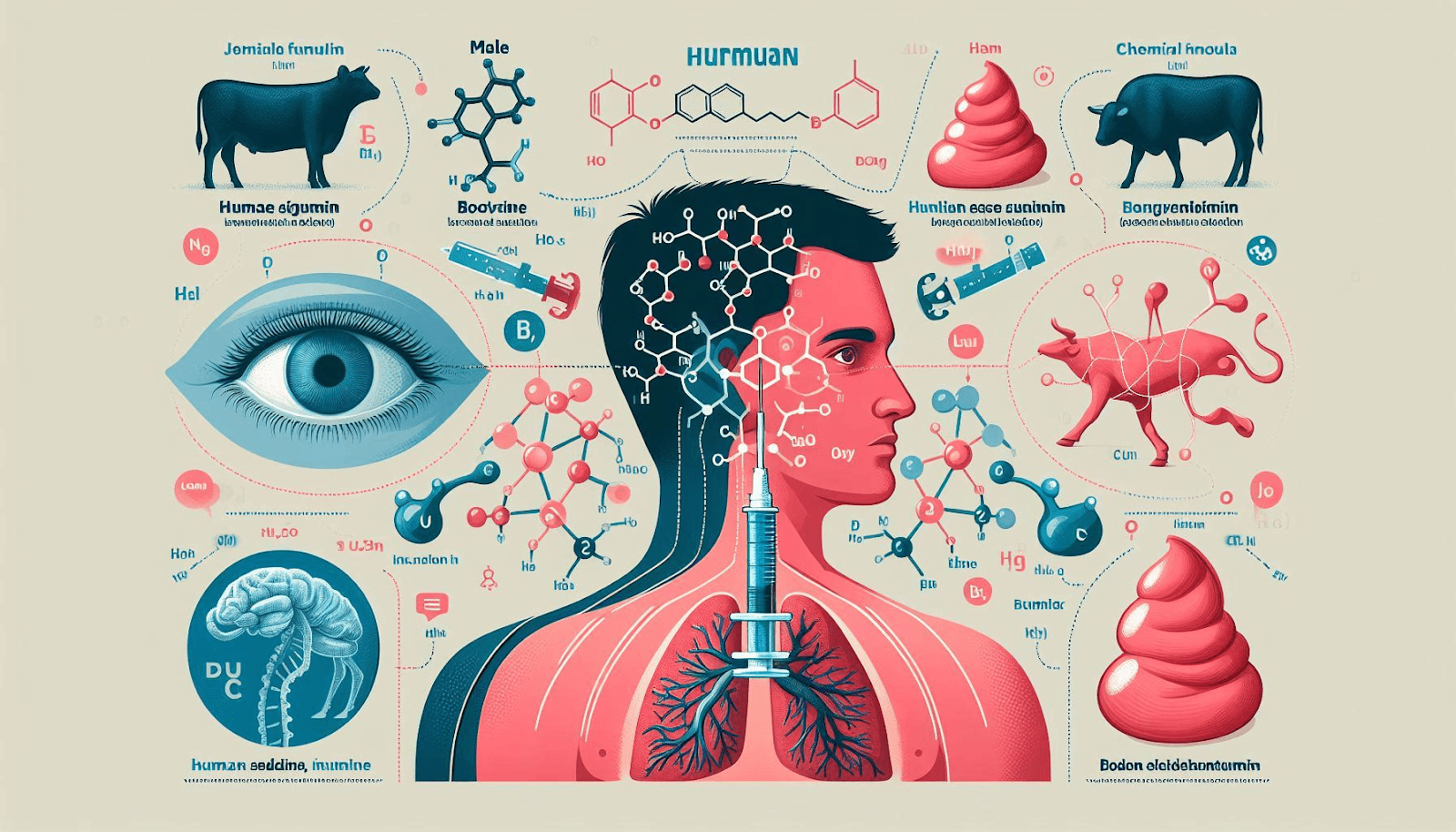
So, are insulin from humans and cows exactly alike? The answer is a resounding no. While human insulin and bovine (cow) insulin share a high degree of structural similarity, there are subtle yet significant differences that can impact their biological activity and therapeutic efficacy.
One of the key differences lies in the amino acid sequence of the insulin molecules. Human insulin consists of 51 amino acids arranged in a specific order, while bovine insulin differs by three amino acids. These seemingly minor variations can influence the way the insulin molecule interacts with receptors on target cells, potentially affecting its potency and duration of action.
Additionally, the manufacturing processes used to produce human and bovine insulin can introduce further variations. While recombinant human insulin is produced through highly controlled and standardized processes, animal-derived insulin may be subject to greater variability due to factors such as the age, diet, and environmental conditions of the source animals.
Despite these differences, it is important to note that both human and bovine insulin have proven to be effective in managing diabetes when used appropriately and under medical supervision. However, the availability and widespread use of recombinant human insulin have largely supplanted the need for animal-derived insulins in most developed countries, driven by improved efficacy, reduced immunogenicity, and the ability to produce human insulin on a large scale through biotechnological processes.
As research into insulin and diabetes treatment continues to advance, scientists are exploring novel approaches to further refine and optimize insulin therapy. This includes the development of insulin analogs, which are synthetic versions of insulin with modified structures designed to improve pharmacokinetic and pharmacodynamic properties, such as faster onset of action or prolonged duration of effect.
While the advent of recombinant human insulin has revolutionized diabetes treatment, the historical contributions of animal-derived insulins, including bovine insulin, should not be overlooked. These early forms of insulin paved the way for the life-saving therapies we have today and continue to play a crucial role in regions where access to recombinant human insulin may be limited or cost-prohibitive.
In conclusion, while human and bovine insulin share similarities in their overall structure and function, they are not exactly alike. The subtle differences in amino acid sequences, manufacturing processes, and potential immunogenicity underscore the importance of ongoing scientific research and the development of increasingly refined and personalized insulin therapies. As our understanding of insulin and its mechanisms of action continues to evolve, so too will our ability to provide optimal diabetes management for individuals worldwide, leveraging the unique properties and advantages of each insulin source.